Ann N Y Acad Sci. 2003 Apr;986:453-60.
Source
Department of Molecular Genetics, Biochemistry, and Microbiology, University of Cincinnati College of Medicine, Ohio 45267, USA. shullge@ucmail.uc.edu
Abstract
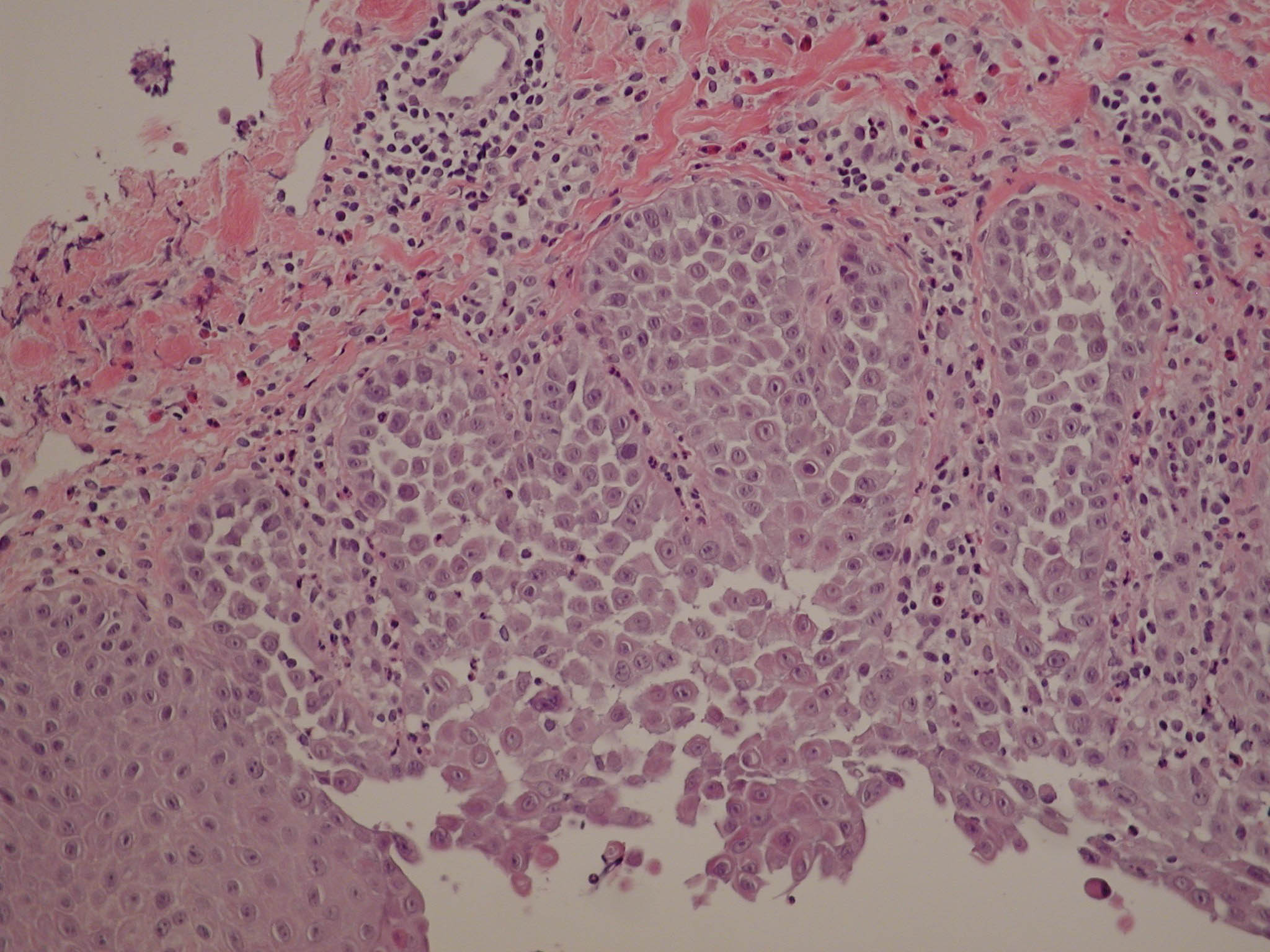
It is known that plasma membrane Ca(2+)-transporting ATPases (PMCAs) extrude Ca(2+) from the cell and that sarco(endo)plasmic reticulum Ca(2+)-ATPases (SERCAs) and secretory pathway Ca(2+)-ATPases (SPCAs) sequester Ca(2+) in intracellular organelles; however, the specific physiological functions of individual isoforms are less well understood. This information is beginning to emerge from studies of mice and humans carrying null mutations in the corresponding genes. Mice with targeted or spontaneous mutations in plasma membrane Ca(2+)-ATPase isoform 2 (PMCA2) are profoundly deaf and have a balance defect due to the loss of PMCA2 in sensory hair cells of the inner ear. In humans, mutations in SERCA1 (ATP2A1) cause Brody disease, an impairment of skeletal muscle relaxation; loss of one copy of the SERCA2 (ATP2A2) gene causes Darier disease, a skin disorder; and loss of one copy of the SPCA1 (ATP2C1) gene causes Hailey-Hailey disease, another skin disorder. In the mouse, SERCA2 null mutants do not survive to birth, and heterozygous SERCA2 mutants have impaired cardiac performance and a high incidence of squamous cell cancers. SERCA3 null mutants survive and appear healthy, but endothelium-dependent relaxation of vascular smooth muscle is impaired and Ca(2+) signaling is altered in pancreatic beta cells. The diversity of phenotypes indicates that the various Ca(2+)-transporting ATPase isoforms serve very different physiological functions.